Juan Brignardello Vela
Juan Brignardello, asesor de seguros, se especializa en brindar asesoramiento y gestión comercial en el ámbito de seguros y reclamaciones por siniestros para destacadas empresas en el mercado peruano e internacional.




A groundbreaking study conducted by Columbia Engineering and the Irving Institute for Cancer Dynamics has unveiled a promising avenue for enhancing cancer treatment in patients with relapsed acute myeloid leukemia (AML). This collaboration with the Dana Farber Cancer Institute (DFCI) has identified a unique population of immune cells that may play a pivotal role in the response to immunotherapy, offering new hope for patients battling this aggressive form of cancer. Acute myeloid leukemia, a disease that strikes four out of every 100,000 individuals in the United States annually, primarily attacks the bone marrow before spreading into the bloodstream. The traditional treatment regimen typically involves targeted chemotherapy followed by a stem cell transplant. Yet, the grim reality is that up to 40% of patients experience a relapse post-transplant, with a disheartening median survival time of just six months. At this juncture, immunotherapy emerges as a critical option for achieving remission. Led by Elham Azizi, an associate professor of biomedical engineering, the research delves into the intricate immune networks present within the bone marrow microenvironments of leukemia patients. This exploration raises crucial questions regarding the variability in patient responses to immunotherapy. Current approaches, such as donor lymphocyte infusion (DLI)—a therapy reliant on donor immune cells—yield a mere 24% five-year survival rate, highlighting the pressing need for more effective strategies. The study reveals that a specific subset of T cells in patients responding positively to DLI may be the linchpin in fighting leukemia by amplifying the immune response. Moreover, it finds that those with a more robust, active, and diverse immune environment in their bone marrow are better positioned to support these cancer-fighting T cells. Employing a proprietary computational technique known as DIISCO, the researchers were able to map the crucial interactions between this unique T cell population and other immune cells. This method, which leverages machine learning to analyze how cell interactions evolve over time, indicated that the success of treatment relies less on the composition of the donor's immune cells and more on the patient’s immune environment. The implications of these findings are profound, suggesting that new interventions could be developed to enhance the immune environment prior to initiating standard DLI treatments. Additionally, the study opens the door to exploring novel combinations of immunotherapies, providing the potential for personalized treatment options for patients who have historically responded poorly to conventional therapies. "This research exemplifies the power of combining computational and experimental methods through close collaboration to answer complex biological questions and uncover unexpected insights," stated Azizi. He emphasized that the findings not only clarify the mechanisms behind successful immunotherapy responses in leukemia patients but also pave the way for developing effective treatments guided by advanced machine learning methodologies. PhD student Cameron Park, who co-led the study alongside Katie Maurer, expressed enthusiasm about the validation of their findings through functional experiments. "This offers real hope for improving cancer immunotherapy," he noted. Looking ahead, the research team aims to further investigate interventions that could enhance the effectiveness of DLI while concentrating on modifying the tumor microenvironment. Despite the excitement surrounding these findings, the team acknowledges that substantial work remains before moving to clinical trials, with the ultimate goal of improving outcomes for patients grappling with relapsed AML. As the landscape of cancer treatment continues to evolve, studies like these illuminate the path toward more effective, personalized therapies.
"Tension Between Trump And Petro Marks A New Chapter In Colombia-U.S. Relations."
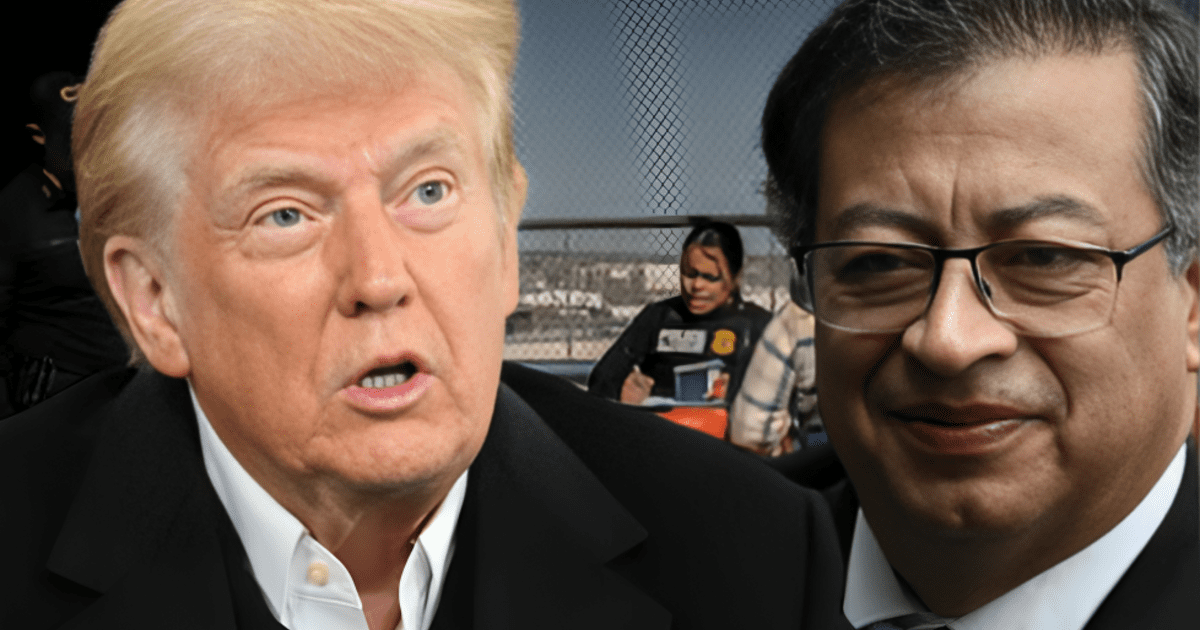
Tensions Between Colombia And The U.S. Rise Due To Tariffs And Immigration Policies.

"Petro Provides Presidential Plane For The Dignified Return Of Colombians."
